You may know someone with breast cancer, or perhaps you are dealing with it now. In either case, you may wonder, “What is breast reconstruction?”
Breast reconstruction surgery aims to restore one or both breasts to near-normal shape, appearance, symmetry, and size.
Women have breast reconstruction surgery following a mastectomy, lumpectomy, radiation treatment, or congenital or developmental breast deformity. Breast reconstruction often involves several procedures performed in stages and can either begin at the time of mastectomy or be delayed until a later date.
There are many breast reconstruction surgery types, and they generally fall into two categories:
- Implant-based reconstruction using implants.
- Flap-based reconstruction using a patient’s tissue from another part of the body.
For multiple reasons, we do not offer flap-based reconstruction alone at PSC, except as a method to save a reconstruction after other procedures have failed.
Let’s Look at Implant-Based Reconstruction
What about implant placement? Above or below the muscle? Which is best? What about mesh in implant-based reconstruction?
Traditionally, reconstruction was performed below the pectoralis and other chest wall muscles. However, this created more elevated, more painful, and less natural-appearing reconstructions.
Patients could also have issues with animation deformity, which is the movement of the implants when the pectoralis muscle contracts. Radiation can be very deforming and painful for these patients as the pectoralis muscle would stiffen over the implant. For this reason, surgeons started using mesh to support the lower part of the reconstruction. So, the trend shifted to place the implant under the pectoralis muscle superiorly but with mesh as support for the lower third of the breast. Many think of this as an “internal bra” holding the implant in place.
Some surgeons then started placing implants on top of the muscles in the place where the breast tissue existed and covered the implant completely with mesh. This is called prepectoral reconstruction. This is usually the best placement for the reconstruction for most patients. Keeping the implant above the muscle decreases post-operative pain and removes animation deformity as a possibility. If the patient has to undergo radiation and the pectoralis stiffens, it does so underneath the implant and thus does not affect the implant as much.
Which Mastectomy Incision is Right for Me?
Mastectomy incisions vary, and the right one for each patient is a decision between the patient, her breast surgeon, and her plastic surgeon. Questions to consider include:
- Do you want your overall breast volume to be the same size, larger, or smaller?
- Are you happy with your nipple position?
For patients who want smaller breasts and are good candidates for breast reduction, we often use a Wise pattern (or anchor incision). This allows us to control the breast skin shape better while making the breast smaller.
Patients who are happy with their nipple position are often good candidates for nipple-sparing mastectomy incisions as long as the cancer is well away from the nipple.
One Stage or Two? Can I Go “Direct-To-Implant?”
Typically, most patients undergo two-stage reconstruction. This means tissue expanders are placed at the time of the mastectomy, and they are used to stretch the skin and soft tissue very gently over a period of weeks until there is enough space for an implant.
This allows the most control over the final reconstruction result. Some patients are candidates for one-stage or direct-to-implant reconstruction. These are often patients who have favorable cancers, are undergoing nipple-sparing mastectomies, and are okay with being the same breast size or a little smaller. Overall, the chance of having a revision surgery is higher if you undergo reconstruction in one stage compared to two.
What Other Adjunct Procedures Are Common with Implant-Based Breast Reconstruction?
Many patients have some rippling at the upper half of the breasts. This can be apparent particularly in pre-pectoral reconstruction as the implant is not hidden by muscle at the upper part of the breast. We treat this with fat grafting and use a small amount of liposuction, usually in the lower abdomen or medial thighs. This fat is then filtered and injected into the upper parts of the breasts under the skin to smooth this area out.
Our plastic surgeons check with the patient’s breast surgeon if the patient had cancer before performing fat grafting to ensure that the fat grafting won’t make it difficult to screen for a cancer recurrence. This procedure is often done at the second stage of reconstruction when the expanders are removed, and implants are placed.
Patients who are not able to have a nipple-sparing procedure may elect to undergo 3D nipple tattooing after their implants are placed. This is covered by insurance and done by our aesthetics team.
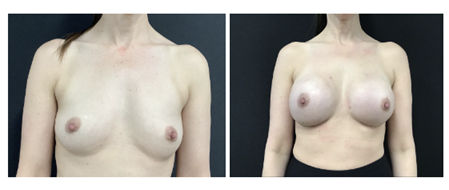
This patient has BRCA2 mutation and underwent nipple-sparing reconstruction in two stages. Her goal was to be larger in volume. She underwent fat grafting at the time of placement of her 605 cc silicone implants.
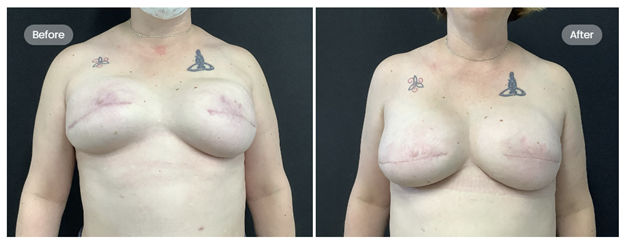
This patient is a good example of a more traditional reconstruction. She had breast cancer treated in Indiana with reconstruction below the pectoralis muscles and mesh for lower pole support. Since her reconstruction, she has suffered from upper arm tightness and a constant feeling of chest muscle strain and chest pain. In her photos, you can see her implants were still quite high, and she has animation with contraction of her chest muscles.
Dr. Spaniol proceeded with the replacement of her previous implants with new implants in the prepectoral position (on top of the pectoralis muscles), with mesh for internal bra support. She is shown eight weeks after surgery, with her implants in a much more natural position and no animation when she flexes her chest muscles. All of her symptoms have resolved, and she is able to sleep comfortably. The next step is 3D nipple tattooing with our aesthetician.

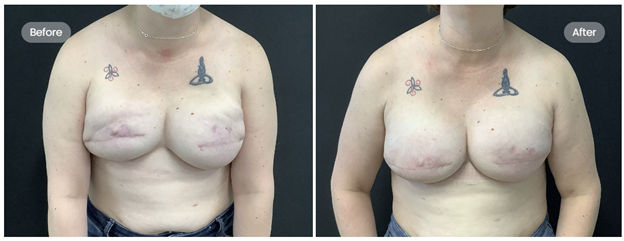
This patient underwent bilateral mastectomy using Wise (anchor-shaped) incisions with placement of tissue expanders and mesh on top of the muscle. She is now shown eight months after her second surgery and has had radiation to her right breast. Next step, 3D nipple tattooing with our aesthetician.

Patients have 3D tattooing as an outpatient, and it is covered by insurance.
The three board-certified plastic surgeons at the Plastic Surgery Center are uniquely qualified to help you with your breast reconstruction. Please contact us at 316-688-7500 for your consultation.
Plastic surgery involves many choices – the most important is selecting a surgeon you can trust. Expect exceptional results when your procedures are performed by plastic surgeons certified by the American Board of Plastic Surgery, like Dr. Sprole, Dr. Biskup, and Dr. Spaniol. These specially trained doctors have at least six years of surgical training and experience, with a minimum of three years of plastic surgery.